 Hi, my name is Emily.
Hi, my name is Emily.
I’m delighted to have been asked to write this week’s blog and for the opportunity to talk about my favourite topic, cardiovascular disease (CVD).
I became interested in CVD as a junior pharmacist working on stroke wards. I remember a man in his 40s who had a huge stroke. He couldn’t move, talk, eat or interact with his loved ones. He lost all his dignity and himself to a disease that is entirely preventable. Stopping others from experiencing the life shattering consequences of CVD is why I do what I do.
We know that people living in our most deprived populations are almost four times as likely to die prematurely of CVD. CVD also contributes to health inequalities for people of ethnic minorities and people with learning disabilities and serious mental illness. We know that the social determinants of health (the conditions in which people are born, grow, live, work and age, which can lead to health inequalities) influence the risk of CVD. Our CVD program is focussed on identifying and treating people at the highest risk in a way that works for them and their health needs.
I went to a CVD prevention conference last October and the most memorable part of the day was a presentation about a patient who’s incredibly challenging life circumstances caused her to die very young of a heart attack. The biases of healthcare workers led to her being dismissed and sent home to die alone when she could have been saved. This goes against everything I stand for and I realised I wasn’t doing enough to stop this from happening. This is what I want to bring to my role as the clinical lead for CVD prevention, I want to do more to tackle the injustice and have this agenda centre stage in everything I do.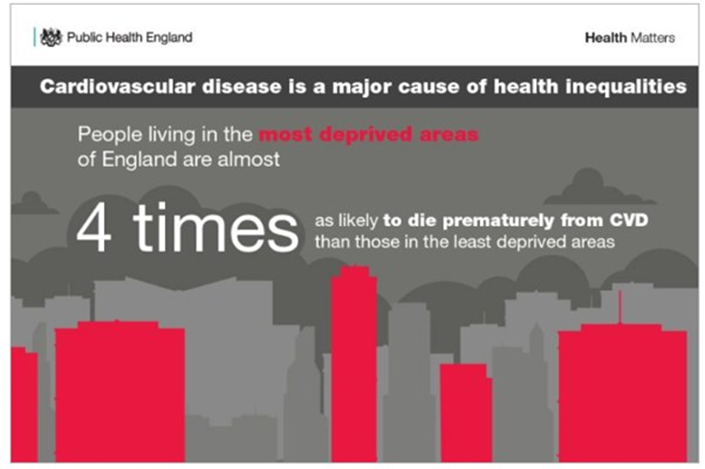
Preventing CVD is not just a job for GP practices. With our partners the Yorkshire and Humber Allied Health Sciences Network, we are working with lots of organisations. Community pharmacies, local councils, hospitals, charity organisations, dentists, research organisations, community leaders, other NHS organisations and many more. Most importantly we will be taking every opportunity we get to engage with our patients, carers and community leaders. The variety of professionals and lay people that can help people reduce their CVD risk has expanded rapidly over the last few years. Everybody needs to come together to tackle this problem.
Over the last few decades we have made huge advancements in reducing CVD deaths. However, over the last few years this has flattened off. We know during the early stages of the COVID pandemic there was a reduction in diagnosis, treatment and monitoring of conditions such as high blood pressure that increase the risk of CVD. In West Yorkshire we are following a national 4-step plan to recover our CVD prevention efforts:
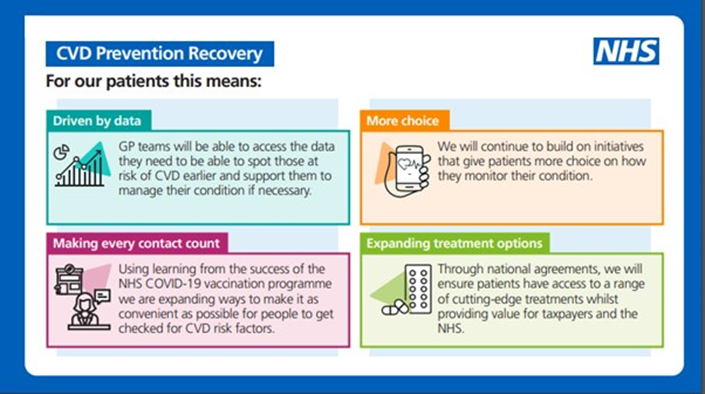
A few examples of the things we will be doing include:
• Making health checks available to people in their community, in a place they feel safe, with people they trust
• Helping GP practices to understand their population better, identify patients at risk of CVD and develop a plan to tackle this problem locally with specialist support
• Working with community pharmacies to help people to access blood pressure checks, stop smoking services, weight management support, and support with medicines that prevent CVD
• Supporting the development of peer leaders; people with lived experience of CVD who are committed to working with us to shape and influence how services are delivered
• Looking for opportunities to better utilise digital health technologies to help reduce people’s risk of CVD
• Helping people to understand their CVD risk and take ownership of their own health through campaigns like ‘know your numbers’
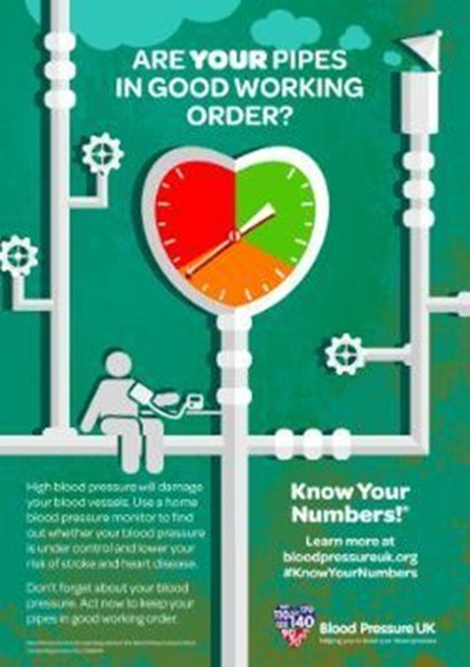
So, what’s the one thing I want everybody to do? Get your blood pressure checked and encourage your family, friends and colleagues to do it too. There are lots of opportunities to do this and we are working on making this more accessible than ever. Most community pharmacies in West Yorkshire offer a blood pressure check service to everybody over 40 or anybody referred by their GP. You can just walk in and ask. If they find your blood pressure is high they can support you with next steps to confirm this, give lifestyle advice and help you get on the right medicines smoothly. This can save so many lives.
If we all work together we can stop ourselves, the people we love, our communities and our patients from dying young or becoming disabled from CVD.
I’d love to hear what you are doing to reduce the risk of CVD, you can let me know on Twitter @EmilyRTurner

