Posted on: 2 July 2021
 Hello, my name is Amanda.
Hello, my name is Amanda.
I am the Matron Lead for Learning Disabilities at Calderdale and Huddersfield NHS Foundation Trust. I want to use this blog opportunity following Learning Disabilities Week to share how much I feel that caring for patients with learning disabilities should not be just for the likes of me in a specialist post it should be for everyone in the NHS.
I’d just like to share two COVID-19 related events here at Calderdale and Huddersfield NHS Foundation Trust which demonstrate our commitment to caring for all – something I am very proud of.
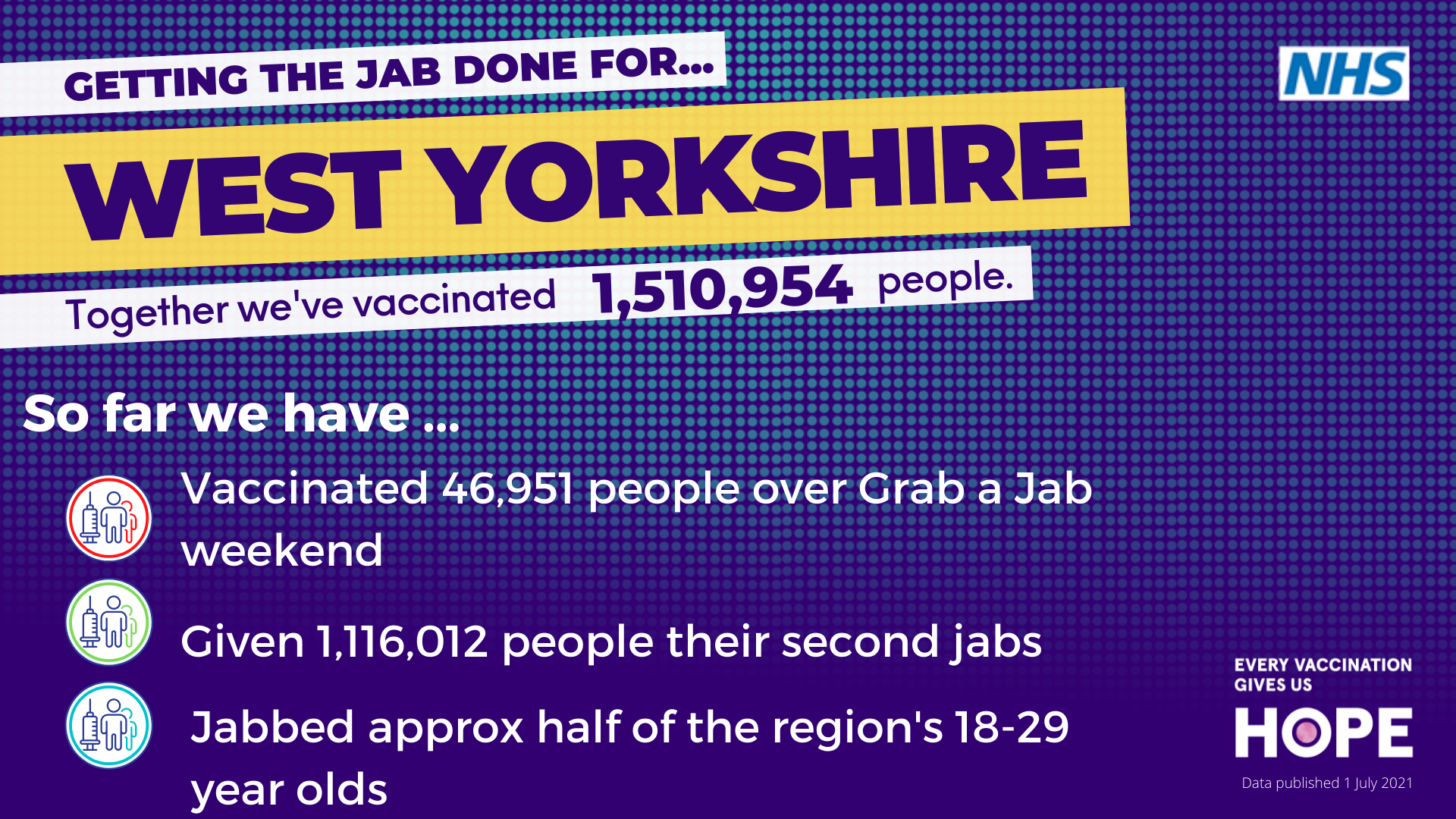
- Our Trust hosted a learning disability COVID vaccination clinic in partnership with South West Yorkshire Partnership Foundation Trust and partner teams in Kirklees and Calderdale. The first clinic we had 83% success rate and second 100%. The feedback was fantastic, many parents felt a sense of relief coming to a clinic where staff understood and made reasonable adjustment. People with a learning disability felt safe and well cared for. The key to success is partnership working, together we can make a difference.
- CHFT is prioritising patients with a learning disability in its reset and recovery work ensuring people on a surgical waiting list are seen in a timely manner. We have a learning disability flag, and this is embedded within its organisational single point of access system called KP+. The Trust can monitor waiting lists and outpatient data for both children and adults with a learning disability and it is working towards an enhanced care pathway for people with learning disabilities.
 I, personally, am celebrating 25 years as a qualified learning disability nurse. I have always wanted to work with people with a learning disability from a very young age and started voluntary work at the age of 14. It’s a real privilege. I am pictured here with colleagues from the Access to Acute group for Yorkshire and Humber (A2A) at the local event held by the University of Huddersfield. I chair the regional A2A and had the pleasure of chairing the conference back in November 2019 which over 100 people attended.
I, personally, am celebrating 25 years as a qualified learning disability nurse. I have always wanted to work with people with a learning disability from a very young age and started voluntary work at the age of 14. It’s a real privilege. I am pictured here with colleagues from the Access to Acute group for Yorkshire and Humber (A2A) at the local event held by the University of Huddersfield. I chair the regional A2A and had the pleasure of chairing the conference back in November 2019 which over 100 people attended.
I met Sheila Hanley at the conference. She came to tell the story of her son Richard who died prematurely. An inquest into his death found there was missed opportunities for potentially life-saving treatment and a lack of coordination amongst the agencies involved. She received a standing ovation and there was many tears and much sadness in the room.
 Paula McGowan is a leading activist calling for mandatory training for all health and social care staff in learning disabilities and autism. She lost her son Oliver and due to her campaign mandatory training for all will be coming in 2022 and called “The Oliver McGowan training”.
Paula McGowan is a leading activist calling for mandatory training for all health and social care staff in learning disabilities and autism. She lost her son Oliver and due to her campaign mandatory training for all will be coming in 2022 and called “The Oliver McGowan training”.
The recent Confidential Inquiry into Premature Deaths of People with Learning disability (CIPOLD 2013 the Learning Disability Mortality Review Programme (LeDer) commissioned by NHS England found issues to address included:
- Fragmented services and poor communication between agencies
- Lack of understanding of the needs of people with learning disabilities
- Negative attitudes and unhelpful assumptions
- Poor compliance with the Mental Capacity Act (2005)
The NHS Plan (2019) made a commitment with specific actions to help tackle health inequalities affecting people with learning disabilities. Specifically, to improve care quality and outcomes, tackle causes of preventable deaths, reviewing referral to treatment, ensuring attendance at outpatients is successful, and reviewing length of stay and readmissions rates within post discharge phase. I have had the privilege of working with my colleagues both here at Calderdale and Huddersfield NHS Foundation Trust and across West Yorkshire and Harrogate Alliance Learning Disability Steering Group on the development of a learning disability awareness E-Learning package. Education and training for all staff is required to ensure we make a difference. So, my ask of everyone is a commitment to undertaking the training package and commit to the Think LD challenge.
 Think LD is the 3 Thinks:
Think LD is the 3 Thinks:
- Think Access
- Think Flexible
- Think Equality
As leaders, how are you going to make a difference?
Have a good weekend everyone.
Amanda
What else has been happening this week?
New Clinical Lead for our Primary and Community Programme
 Dr Steve Ollerton has been appointed as the new clinical lead for the West Yorkshire and Harrogate Health and Care Partnership Primary and Community Programme.
Dr Steve Ollerton has been appointed as the new clinical lead for the West Yorkshire and Harrogate Health and Care Partnership Primary and Community Programme.
Steve brings with him a wealth of expertise and experience. He has been GP partner at Skelmanthorpe Surgery in Huddersfield since 2003, nurse practitioner trainer from 2004-2007 and a Practice Based Commissioning board member from 2008-2012.
Steve was also Chair of Greater Huddersfield Clinical Commissioning Group from 2013 to 2021 and sat on the Yorkshire and Humber Clinical Senate from 2014 to 2018 when it finished. Other roles include being a member of NHS Clinical Commissioners since 2018.
Carol McKenna, Chief Officer for Kirklees Clinical Commissioning Group and Senior Responsible Officer for the Primary and Community Programme said:
“We are delighted to have been able to offer Steve the post of primary care clinical lead and are very happy he has accepted. The role is extremely important with immediate priorities that include supporting programme board members to establish the West Yorkshire Clinical Director Reference Group, whilst advising and providing leadership on the future direction of the board at this critical and challenging time.”
Steve said:
"I am really pleased to be joining the progamme and working with the primary and community care team. This is a crucial time for primary care to evolve in our post pandemic world. I look forward to offering guidance to our clinical directors and ensuring our primary care networks achieve their potential working with their partners in their networks. I am also looking forward to being a strong clinical voice within our integrated care system."
Future Design and Transition: Chairs and Leaders Reference Group
 Group members include council leaders and NHS Trust Chairs. Members meet once a month to receive an update on the progress we are making towards the NHS legislation proposals for integrated care systems like our Partnership. The group is co-chaired by Cllr Tim Swift, Chair of our Partnership Board and Cathy Elliott Chair of Bradford District Care NHS Foundation Trust.
Group members include council leaders and NHS Trust Chairs. Members meet once a month to receive an update on the progress we are making towards the NHS legislation proposals for integrated care systems like our Partnership. The group is co-chaired by Cllr Tim Swift, Chair of our Partnership Board and Cathy Elliott Chair of Bradford District Care NHS Foundation Trust.
There was a discussion around the pressure facing all sectors, for example accident and emergency departments, primary care and social care and the importance of communicating with people across the area regarding the most appropriate place for help to ensure it meets their needs. Health inequalities was also covered, including the work we are doing to address inequalities for people with learning disabilities and race equality. The success of the West Yorkshire Vaccine Programme was also discussed ahead of the ‘Grab a Jab’ weekend, last week.
Members received an update on ‘Our People’ ambition which is to make West Yorkshire and Harrogate ‘a great place to live and work’ for our One Workforce across all areas of health and care, including voluntary community social enterprise sector. Members also received an update on the development of our Partnership constitution which will build on our existing memorandum of understanding. There was also a conversation on ‘what good governance looks like’.
Innovative companies selected for green accelerator programme to help tackle the NHS’ carbon footprint
 A sustainable 3D printer, a digital personal health record and an integrated care platform connecting patients and healthcare professionals are the products that will be the focus of Yorkshire & Humber Academic Health Science Network’s (AHSN) inaugural ‘green’ accelerator programme.
A sustainable 3D printer, a digital personal health record and an integrated care platform connecting patients and healthcare professionals are the products that will be the focus of Yorkshire & Humber Academic Health Science Network’s (AHSN) inaugural ‘green’ accelerator programme.
Commissioned by West Yorkshire and Harrogate Health and Care Partnership and delivered by Yorkshire & Humber AHSN, the Propel@YH Net Zero pilot programme will provide companies Automedi, Patients Know Best and Dignio with access to a structured course of bespoke support and advice around the environmental sustainability of their products.
Community providers
On Monday, the Chairs and CEOs from organisations across West Yorkshire who provide community NHS services met for an exploratory discussion on bringing together a collaborative community health system partnership. Strong community health services are at the heart of improving the health and wellbeing of our population, and play a key role in enabling the wider integration of services at home and close to home, working together with primary care, secondary care, social care and the voluntary community social enterprise sector. Colleagues discussed what a community provider collaboration might look like, potentially along the lines of a ‘learning and development’ network and one that can deliver an outcome that exceeds the sum of the parts.
Older People Housing
 A task and finish group has been set up as part of our Improving Population Health Programme, to focus on the delivery of actions to support older people housing. It will meet monthly. A subset of the Housing for Health Network led by John Ebo, Assistant Director for Improving Population Health, the group brings together broad perspectives and experience from across our Partnership.
A task and finish group has been set up as part of our Improving Population Health Programme, to focus on the delivery of actions to support older people housing. It will meet monthly. A subset of the Housing for Health Network led by John Ebo, Assistant Director for Improving Population Health, the group brings together broad perspectives and experience from across our Partnership.
The group has representation from Care and Repair England, and housing from across our local places as well as the Centre for Ageing Better, West Yorkshire Combined Authority and the voluntary and community social enterprise sector. Group members will focus on:
- Development and delivery of an awareness raising campaign to promote sheltered housing across West Yorkshire and Harrogate.
- Identifying and sharing good practice on emerging technology and digital strategy
- Identifying and sharing good practice on incentive schemes.
System Oversight Assurance Group
The Partnership’s System Oversight and Assurance Group (SOAG) met last Friday. This group has been established to take an overview of progress with our shared priority programmes, and to agree collective action to help tackle shared challenges. In this meeting the group discussed the five-year plan ambitions and how we measure the progress we are making for people and communicate this easily.
Healthwatch colleagues also give an update on their work to hear the voice of people, and particularly those with a hidden voice. Hearing the voice or experience of people living in care homes has been part of the work of every local Healthwatch and a priority area for several local Healthwatch organisations. Healthwatch Wakefield have worked closely with the Wakefield Safeguarding partnership, report as attached in appendix. Healthwatch Kirklees had done significant pre-COVID work looking at the GP offer into Care homes. Healthwatch Leeds, working closely with Carers Leeds, have undertaken a focused piece of work since May 2020 to hear and highlight the experiences of care home residents and their families. This has been particularly focused on the ongoing significant and devastating impact of severely restricted family contact and periods of isolation.
Forget Me Not Children Hospice
Forget Me Not Children Hospice receive a video message from their royal patron, HRH Princess Beatrice as part of Children Hospice Week (last week).
Thank you to our royal patron, HRH Princess Beatrice, for this wonderful message of support as we approach the end of #ChildrensHospiceWeek pic.twitter.com/YEJQK0EIcG
— ForgetMeNotChildren (@ForgetMNotChild) June 27, 2021
Enhancing virtual care capabilities for children and adults
 Another project highlighted in the Yorkshire & Humber Health Academic Science Network (AHSN)’s Impact Report is TytoCare. TytoCare was piloted first in the paediatric department at Bradford Teaching Hospital, with its use adapted in response to the pandemic. TytoCare have developed a wireless, handheld examination device that allows users to perform medical examinations anytime, anywhere, for the ear, throat, lungs, heart, temperature, skin, and abdomen. These examinations can be on-line, live with a medical professional, or can be recorded by the patient, parent or carer and uploaded to a secure platform for review by the clinical teams.
Another project highlighted in the Yorkshire & Humber Health Academic Science Network (AHSN)’s Impact Report is TytoCare. TytoCare was piloted first in the paediatric department at Bradford Teaching Hospital, with its use adapted in response to the pandemic. TytoCare have developed a wireless, handheld examination device that allows users to perform medical examinations anytime, anywhere, for the ear, throat, lungs, heart, temperature, skin, and abdomen. These examinations can be on-line, live with a medical professional, or can be recorded by the patient, parent or carer and uploaded to a secure platform for review by the clinical teams.
Yorkshire & Humber AHSN are working with TytoCare to help spread the adoption of this innovative device in a variety of care settings from helping ventilated patients at home to emergency
departments to care homes. So far, 14 healthcare organisations across our area have adopted this device. Leading and managing the implementation centrally via the AHSN has removed duplication of effort (e.g. for procurement), optimised preparations for benefits realisation and ensured that implementation is robust.
Yorkshire & Humber AHSN is one of 15 AHSNs set up by NHS England to operate as the key innovation arm of the NHS. The organisation helps ensure new innovative products and services that have the potential to transform lives become part of routine clinical practice.
Join the Anti-Racism Movement and share with your network
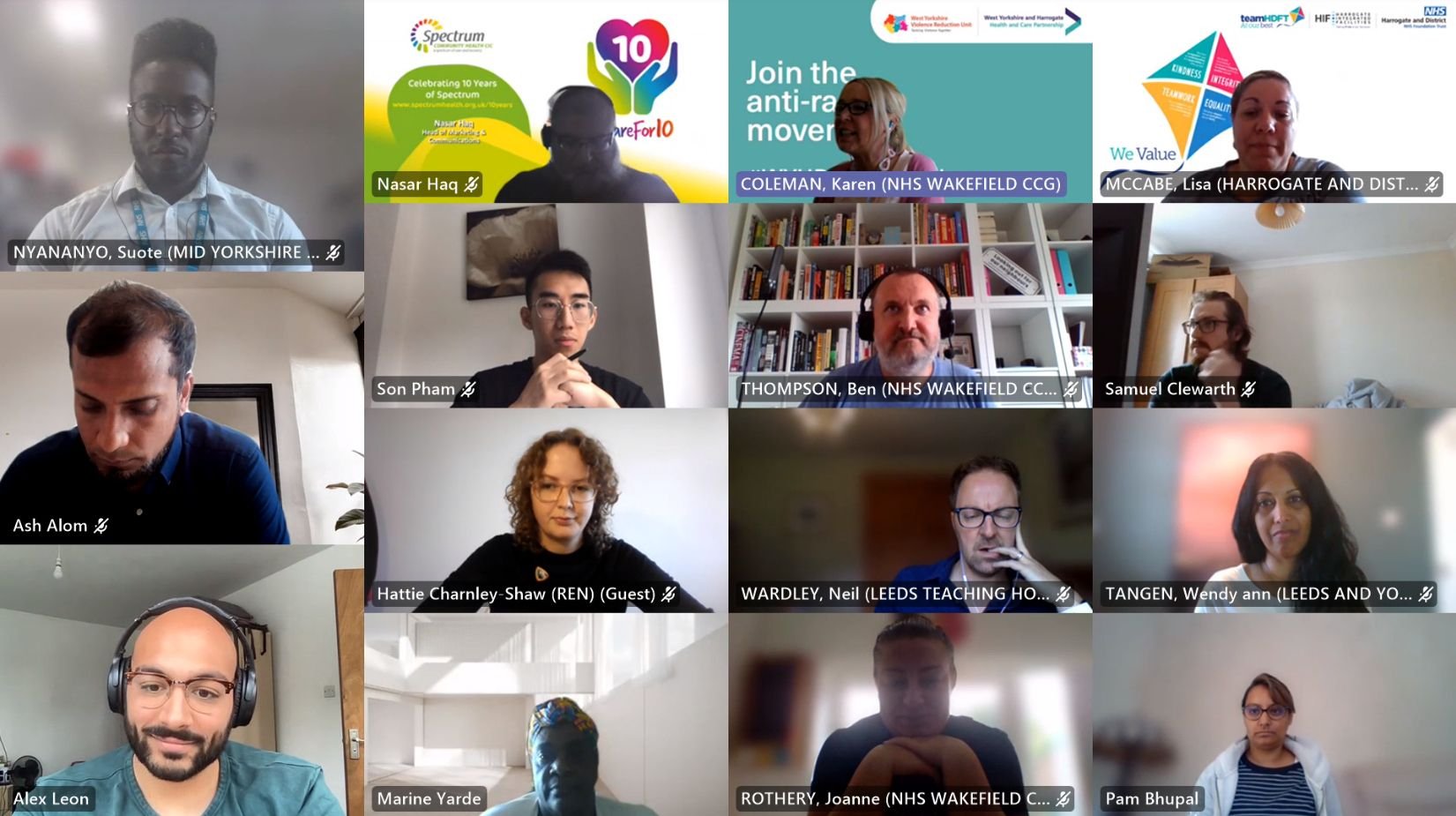 Together with the West Yorkshire Violence Reduction Unit (VRU) we are launching the anti-racism movement at the end of August and are delighted that more than 300 organisations have pledged their support, including leading sports clubs.
Together with the West Yorkshire Violence Reduction Unit (VRU) we are launching the anti-racism movement at the end of August and are delighted that more than 300 organisations have pledged their support, including leading sports clubs.
Paul Mitchell, Bradford Bulls Foundation said: “Sports clubs and foundations have the perfect platform to make a positive difference for everyone in our region who has ever suffered from health inequalities. As a Rugby League Foundation, we strive to make all of our activities reflect this. However, there is so much more to be done to ensure real, permanent change which cuts across all aspects of society and its institutions. This can only be achieved through a concerted effort, so we welcome and fully back this important initiative”.

Jake Webster, a New Zealand international rugby league footballer who plays as a centre for the Keighley Cougars said: "Here at Keighley Cougars we celebrate individual stories for example, age, gender, race and sexuality. We encourage our workers/players to ask questions and speak to others to understand different cultures. Coming from a different country I have seen racism from a different perspective and understand the problems it can cause. We hope to create opportunity and pathways for everyone."
Craig Shepherd, Wakefield Trinity Community Foundation said: “As a charity situated within the sporting world we unfortunately encounter racist behaviour, regularly, and do our best through messaging, whether through the assemblies we deliver in schools or the projects we deliver in communities, to raise awareness and educate. We are delighted to back the campaign and would encourage our network and supporters to do so as well so that we can tackle the issue of racism in society”.
John Mallalieu, CEO at the Leeds United Foundation said: "The Leeds United Foundation are thrilled to be a part of this important campaign striving to make a positive difference for those in our community. We deliver various educational activities around the importance of Equality, Diversity and Inclusion and the fact that racism continues to affect so many people in a negative way, on a daily basis, means that we must continue to raise awareness, fight for equality and support initiatives such as this. To see so many organisations involved is incredibly important, by working together we have the best opportunity to really make a difference."

Please get involved in this important, meaningful, and powerful movement developed with colleagues by registering your support at https://
MyCare24 set to be largest service of its kind in England
Following a successful trial during COVID-19, thousands of people with long-term respiratory conditions across Bradford District and Craven are set to receive support through a dedicated remote monitoring app with over £400,000 being invested by NHS England.
Thanks to the cash boost over the next two years a total of around 6,000 people with chronic obstructive pulmonary disease (COPD) will get help to manage their condition through a specially designed app. This follows a successful trial involving 50 people recovering from COVID who have been using an app called Luscii as part of the district’s Act as One Respiratory Programme. During the trial people had round-the-clock access to the MyCare24 clinical team, using the remote monitoring app to recognise when oxygen levels begin to deteriorate.
The funding will now mean people with moderate through to those with severe respiratory conditions will be given access to the app or a paper-based version of the app for those unable to use smartphones.
Chronic obstructive pulmonary disease (COPD) is the name for a group of lung conditions that cause breathing difficulties. The breathing problems tend to get gradually worse over time limiting normal activities, although treatment and self-management can help keep the condition under control.
New licensing initiative set to boost safety and security for staff, customers and local communities
 A new pioneering licensing initiative to help provide safe and secure bars, pubs, clubs, restaurants and hotels across Bradford, Calderdale, Kirklees, and Wakefield launched this month.
A new pioneering licensing initiative to help provide safe and secure bars, pubs, clubs, restaurants and hotels across Bradford, Calderdale, Kirklees, and Wakefield launched this month.
The Licensing Security & Vulnerability Initiative (SAVI) is an online and confidential self-assessment tool which brings together the guidance, standards and advice that is provided by police and local authority licensing officers and other responsible authorities. The West Yorkshire and Harrogate Health and Care Partnership together with West Yorkshire’s Violence Reduction Unit commissioned the Home Office backed initiative in agreement with partners from the West Yorkshire Public Health Reducing Violent Crime Network.
For more information please contact emmerline.
Evaluating digital access to general practice
 Around 60 primary care colleagues, including from GP practices, joined an online workshop on 23 June 2021 to share their experiences of using GP online consultation, video consultation and SMS text messaging.
Around 60 primary care colleagues, including from GP practices, joined an online workshop on 23 June 2021 to share their experiences of using GP online consultation, video consultation and SMS text messaging.
The event helped to get a better understanding of what support practices need from the Digital Programme to improve effectiveness and efficiency and provided an opportunity to share best practice. The information will also feed into the next round of procurement of these tools to ensure that we develop a service specification which will deliver the products of most benefit to primary care. For more information and copies of the presentation see the news pages on our website.
Red Kite View
 The bi-monthly West Yorkshire Children and Young People’s Mental Health (formerly known as CAMHS) Inpatient Service stakeholder newsletter includes the latest development of the new Red Kite View inpatient unit due to open in December 2021 in Leeds for West Yorkshire young people who need specialist support.
The bi-monthly West Yorkshire Children and Young People’s Mental Health (formerly known as CAMHS) Inpatient Service stakeholder newsletter includes the latest development of the new Red Kite View inpatient unit due to open in December 2021 in Leeds for West Yorkshire young people who need specialist support.
The site is now completely unrecognisable as the area has evolved. Progress on the build is going well and it’s incredible to see the images from the architect’s impressions being brought to life.
Accelerating the future of healthcare with better remote care options for babies with cleft lip and palate
Parents travelling long distances to see a surgeon to agree options for new-borns with cleft lip and palate could be a thing of the past, thanks to new technology connecting clinicians with patients and families in their own homes. Leeds Children’s Hospital is trialling the virtual consultation and remote imaging capabilities of the TytoCare digital solution, in partnership with the West Yorkshire and Harrogate Health and Care Partnership, NHSX and the Yorkshire and Humber Academic Health Service Network.
Emma Blair, lead nurse for the cleft lip and palate service at Leeds Children’s Hospital explained: “To agree surgical options for children with a cleft lip and / or palate, and review postoperative healing, consultants need a high-quality view of the inside of the mouth. Currently, we can only do this by seeing the patient face to face at the hospital. However, Tyto’s virtual capabilities, which includes a hand-held assessment tool, means the nurse can visit the patient’s home to capture high quality images to share with the surgeon and plan surgical care options. “Clinical nurse specialists obtain postoperative images and share these with the surgeon to review post-operative healing. At the moment, the surgeon has to see the patient face to face to do this. Using Tyto technology means we can provide high quality images that enable better-informed remote clinical decision making.”

